현재 사용 중인 언어로는 이 페이지를 사용할 수 없습니다. Google Translate을 사용하여
자동 번역된 페이지
를 볼 수 있습니다. Renishaw에게는 이 서비스를 제공할 책임이 없으며 번역 결과를 저희가 확인하지도 않았습니다.
추가로 도움이 필요하시면
저희에게 연락해 주십시오.
Mission to Nepal – surgical education and innovation in disaster affected regions
The disastrous Nepal earthquake of 2015 left the health and surgical care systems of the country in disarray. To support and train local surgeons, a team of UK specialists undertook three missions to the country. Following the first mission a patient who suffered a road traffic accident was brought to their attention, culminating in what is believed to be the country's first customised 3D printed orbital implant.
Background
Shashi Kala Rai is a young mother, aged just 28, who received ground-breaking surgery at the expert hands of consultant Oral and Maxillofacial Surgeon Shakir Mustafa, in Dharan. The young woman was one of several patients he treated during two aid and education mission visits. She had sustained an orbital floor and medial wall fracture in a road traffic collision.
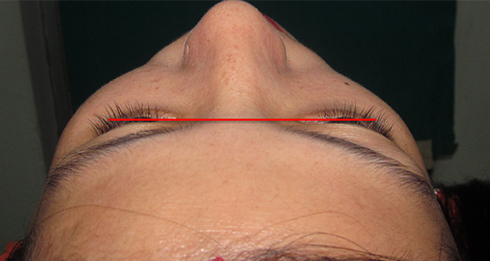
Rai had previously funded her own corrective bone graft surgery in India but was left with unequal eyes. The left eye was lower, sunken-in and scarring had reduced its size. Her left eyelids needed to be revised laterally and the eye supported and re-aligned.
Life started to feel better once she came under the care of Mustafa, a busy surgeon who chairs the Norman Rowe International Education Foundation (NRIEF), a subcommittee of The British Association of Oral and Maxillofacial Surgeons' (BAOMS), the body responsible for running this mercy mission.


Scrutinising hard copies of her CT scans, Mustafa could see that the bone graft was incorrectly placed and lying partly in the maxillary sinus and only partly in the orbit. He was convinced that he could significantly improve Rai's condition.
After returning to the United Kingdom, Mustafa began planning the operation. He enlisted the help of local colleagues at the cutting edge of patient specific solutions and introduced the power of digital processes into his pre-surgical planning.
The surgeon collaborated with a team of experts in 3D design and printing who had a track record of supporting predictable results in complex facial reconstructive surgery. Renishaw plc was enlisted in the project as the metal 3D printing supplier. As one of the world's leading engineering and scientific technology companies, Renishaw also contributed its precision measurement skills to produce the complex geometries needed to help the implant fit perfectly, first time. Renishaw also donated the implant and offered financial support.
I am always ready to modify the operation to suit local conditions, but I will never compromise my standards and I always plan for perfection includes the implant which fitted perfectly.
Shakir Mustafa (Oral and Maxillofacial Surgeon)
Challenge
Orbital implant procedures always carry the risks of causing blindness or double vision, because of the position of the optical nerve. In the NHS, such operations are always left to the most experienced surgeons. As the lead on maxillofacial trauma with special interest in orbital surgery, Mustafa handles all orbital reconstruction procedures for Cwm Taf University Health Board, South Wales.
In this case, there were the added risks from being a secondary reconstruction procedure, with earlier incisions and scars jeopardising his ability to restore full form and function. Despite these challenges, this would be an operation where a customised orbital floor implant would make a world of difference and support a predictable outcome with reduced risks.
While the UK has over 1,000 Oral and Maxillofacial surgeons of all grades, Nepal has fewer than 50, so this mission to Nepal was designed to leave an added legacy of teaching support.
The Indian sub-continent has a particular problem with oral cancer, which is 20-30 times more prevalent than in the UK. The challenge of the training part of this mission was to kick-start a medical teaching programme, training local surgeons and physicians from multiple disciplines of hospital medicine to treat trauma and oncology patients.

Solution
Mustafa worked with Peter Evans and Heather Goodrum at Morriston Hospital's Maxillofacial Prosthetics Laboratory in Swansea to design the implant in computer-aided design (CAD), with the plates to be visualised and edited in a 3D virtual environment using a haptic arm.
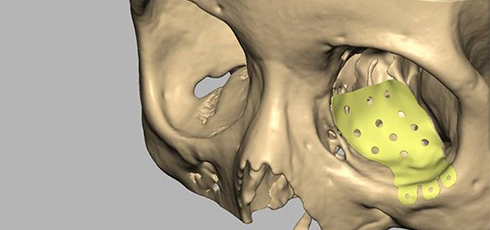
Mustafa suggested clinical design modifications, using the flexibility of the process to compensate for the defects from Rai's first operation, where scar tissue and an ill-fitting bone graft could potentially undermine the plate's chances of a good fit.
The plate needed to cover the existing orbital floor and medial wall defects. The team also made adjustments on screen to increase the venting holes, thus aiding drainage. They reduced the extension to the rear of the plate to avoid the optic nerve and reduced the extension of the plate up the medial wall to make surgical placement easier and more predictable.
The earlier fracture had allowed some orbital fat to herniate down in to the maxillary sinus resulting in a sunken eye appearance. To compensate, an exaggerated curvature was added to the plate to recreate the retrobulbar bulge of the eye socket and give added aesthetic benefit.
Finally, an anatomical model was printed by PDR at the Cardiff Metropolitan University in stereolithographic resin, a material that can be sterilised, so allowing the model to be taken into theatre to further help the surgeon during the operation.
The .stl files were sent to Renishaw's new state-of-the-art additive manufacturing facility in nearby Miskin, where an implant was produced on Renishaw's AM250 machines. Renishaw's digital workflow ensured the company was able to deliver the implant printed in the proven titanium Ti MG1 material which is tested to ISO 10993 part 1.
Only one implant was needed, but a second implant was manufactured using traditional techniques at the Maxillofacial Unit, Morriston Hospital as a form of insurance, given the scale of the journey and the volatility of the region after the earthquakes.
After an overnight flight from the UK, Mustafa operated within hours of arrival, unpacking only his medical equipment and the precious implant. He knew this would give his patient maximum time to recover before his return flight, letting him assess the results of surgery and request post-operative CT scans if needed.
The operation was a success, despite the many challenges facing him, because Mustafa applied his guiding belief system in “planning to perfection”.
Mustafa had taken everything he needed, including his own supply of diathermy tips and patient return electrode earth pads. He took his own head lamp, a standard item in these procedures, but vital in the post-earthquake environment where aftershocks and electrical power cuts could be expected in surgery.
“I am always ready to modify the operation to suit local conditions, but I will never compromise my standards and I always plan for perfection,” said Mustafa. “That includes the implant which fitted perfectly.”
Our aim is to lay down the foundations for a future training programme through empowering local faculty to take charge of the education and training of future generations of Nepalese surgeons.
Shakir Mustafa (Oral and Maxillofacial Surgeon)
Results
This operation is believed to have been a first in many ways in Nepal: the first customised maxillofacial operation and the first 3D printed orbital implant surgery of any kind.
The operation took twice as long as it would have taken in the UK, due to local conditions. There were four clinicians in the operating theatre and the procedure was watched by Nepalese and UK trainee surgeons, who assisted and observed for training purposes.
By the time Mustafa left Nepal, Rai was still slightly swollen from her operation, but once the sutures were removed, she had normal visual acuity, no double vision, good eye and eyelid movement and the correct eye position had been restored. She made a full recovery and was delighted with the results.
Mustafa has set up a five-year collaboration for this training. He said: “Our aim is to lay down the foundations for a future training programme through empowering the local faculty to take charge of the education and training of future generations of Nepalese surgeons.”