Digital evolution of cranial surgery
From complex reconstructive facial surgery to orthopaedic and trauma surgery, advances in additive manufacturing have inspired a growing number of progressive surgeons to commission metal 3D printed patient specific implants (PSIs) and cutting guides for both complex and straightforward procedures.
Case studies are emerging which provide compelling evidence that the surgeons embracing this technology over standard implants or traditionally manufactured implants are consistently delivering better and more predictable outcomes, in terms of patient safety and satisfaction, and hospital efficiencies and economies.
UK NHS hospitals, in their quest for better quality and efficiency, have used 3D-printed anatomical models, guides and implants to improve the predictability, accuracy, safety and speed of operations.
A hospital in Spain has proved that the technology can also be used across international borders in a classic example of global technology transfer with UK experts.
Case presentation
Neurosurgeon Bartolomé Oliver, MD, PhD, practises at the Teknon Medical Center in Barcelona, Spain and has trained internationally including in Canada, USA and Sweden.
A 68-year-old female patient presented to his department with a benign growth from the left side of her cranium, caused by a meningioma, a tumour that arises from the meninges – the membranes surrounding brain and spinal cord.
The computerised tomography (CT) scan revealed the growth was expanding outwards into the skull-bone. The patient required a craniectomy to remove the growth and a cranioplasty to rebuild her skull.
Dr Oliver planned for the combined craniectomy and cranioplasty operation allowing the patient to be treated in a single procedure. He knew the operation should not present any challenging problems, but his priority was to ensure it gave the best results to both patient and hospital. He chose to partner with UK experts in 3D design and printing who had shown repeated evidence of supporting predictable outcomes in complex facial reconstructive surgery.
Design
Dr Oliver briefed PDR, a world-leading design consultancy and applied research centre, based in Cardiff, UK, to design both a PSI cranial plate for the cranioplasty and a custom surgical cutting guide for the craniectomy. The 3D metal printing partner was Renishaw plc, one of the world's leading engineering and scientific technology companies with expertise in precision measurement and healthcare.
The hospital's CT scans were transferred from Spain to the UK, imported into MIMICS® software program at PDR's offices, and then converted into an .stl file for modelling by PDR.
PDR created a 3D virtual model of the cranial plate by mirroring the healthy side of the cranium using Geomagic® Freeform® Plus software to deliver a good aesthetic design.
PDR also modelled the cutting guide which would be placed on the cranium to help mark the perimeter or limit of the craniectomy and act as an aid in freehand work during surgery. The initial designs were sent back to Dr Oliver for first review. It then only took a 40 minute Skype™ session with Dr Oliver, PDR and Renishaw's Spanish representative, for the surgeon to share his design modifications.
Manufacturing
Renishaw received the files of the approved designs for both the implant and cutting guide and 3D printed them at its central manufacturing unit in Stonehouse, UK, despatching the components to Barcelona within two weeks of receiving the files.
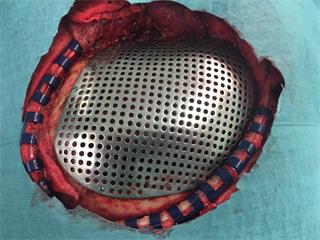
The parts were manufactured on a Renishaw AM250 metal 3D printing machine in titanium with a satin finish as per Dr Oliver's specification. The material used was Ti MG1 tested to ISO 10993 part 1, which was then treated with Renishaw's X-flex™ technology. This ensures high ductility, which is important to prevent the risk of breakages in surgery should the implant need to be adjusted, for example due to unexpected hard tissue changes.
Ensuring an excellent aesthetic outcome meant that the contoured cranial plate needed to match the patient's cranial contours accurately.
While the virtual modelling enabled precision design, the plate needed to be thin enough to maintain aesthetics, but resilient enough to handle all of the other necessary requirements: additional screw holes to give Dr Oliver flexibility to fix the implant and perforations to allow fluid transfer and tissue to grow through it.
The implant extended 8 mm past the cut margin – giving an 8 mm offset allowed for cutting tool radius and standard screw diameter - and was designed for 1.55 mm diameter screws. This design freedom enabled by the additive manufacturing process meant that the material was thicker around the screw holes but 0.5 mm overall, to fit Dr Oliver's precise specification.
Operation
Dr Oliver had specified that a “pan-handle” be designed into the cutting guide to help position it during the craniectomy, aiding stability and improving the ergonomic performance of the device. An arrow was added onto the guide to indicate the orientation.
The decision was taken to use the cutting guide to mark the perimeter of the craniotomy. Dr Oliver executed a freehand incision following the markings, after the guide was removed. This approach enabled an easier way to handle the complex skull geometry around the temporal area which curved to a tight radius.
With additional redundant screw holes, Dr Oliver was able to operate with maximum discretion, due to his design. He had specified more fixation options in the event that he needed to adapt at short notice. The operating theatre is a characteristically changeable environment and it pays to guard against possible mishaps. The implant gave him that additional safety factor.
The operation was successful and incident-free with the cranial plate being fitted safely and accurately.

Parts were delivered to us according to plan which allowed us to prepare them for the surgery. No adjustment was needed during surgery. Using the 3D-printed cutting guide and implant saved us approximately 30 per cent of the time required for this kind of surgery.
Neurosurgeon Bartolomé Oliver, MD, PhD (Spain)
Post surgery
The patient was discharged after four days in hospital and examined in follow-up appointments after 15 days and at monthly intervals. She was free from complications. Post-operative CT scans showed good implant performance.
Describing the main benefits for the patient, Dr Oliver mentioned “the excellent aesthetics offered by this implant” adding that “the patient is very happy with it”.
Conclusions
A relatively routine operation to remove a tumour has proven three main benefits of being able to make a PSI to the surgeon's design: safety, patient satisfaction and savings in surgery time.
With safety being the paramount priority, supplying a predefined cutting guide and the corresponding implant helped eliminate all the risk that might come from the freehand work of the procedure. Dr Oliver's own verdict: “It ensured an absolutely safe operation with no risk to the patient.”
Patient satisfaction was also a priority and the precision of the PSI enabled the surgeon to provide the aesthetic quality needed. As with more complex facial reconstruction procedures, the power of patient-specific design provided added dimensions of consistency and predictability.
A 30 per cent saving in theatre time was the third benefit of this streamlined method.
As Dr Oliver noted, “Parts were delivered to us according to plan which allowed us to prepare them for the surgery. No adjustment was needed during surgery. Using the 3D-printed cutting guide and implant saved us approximately 30 per cent of the time required for this kind of surgery.”For his worldwide peers Dr Oliver believes his approach offers a good model. He comments, “Working with precise products and good planning is very positive and recommendable.”
The 30 per cent time saving has huge significance for hospital management and health economists where theatre time is costed by the minute. Therefore every minute saved can offer substantial cost savings for healthcare providers.
Additionally, shorter surgery times can help reduce infection risk, accelerate the patient's recovery and allow for higher theatre throughput.
The digitised workflow connecting design experts, surgeons and manufacturing illustrates the power of global technology transfer and international co-operation. It has the potential to democratise technology by giving any hospital, in any corner of the world, access to precision technology, products and materials.
Note: All brand names and product names used in this document are trade names, trade marks or registered trade marks of their respective owners.