Ta strona nie jest obecnie dostępna w Twoim języku. Możesz zapoznać się z tłumaczeniem automatycznym, korzystając z usługi Google Translate. Nie jesteśmy odpowiedzialni za świadczenie tej usługi, ani też wyniki tłumaczenia nie były przez nas sprawdzane.
Jeżeli chciałbyś uzyskać więcej pomocy skontaktuj się z nami.
World leading epilepsy surgery centre in Milan uses Renishaw’s stereotactic robot
The neurosurgeons at the Claudio Munari Epilepsy and Parkinson Surgery Centre of the Niguarda Hospital in Milan, Italy, use the Renishaw neuromate® stereotactic system in stereoelectroencephalography (SEEG) procedures to define the epileptogenic zone. The team reports increased accuracy and a reduction in surgery time, with a very low complication rate.
Introduction
Dr. Francesco Cardinale, one of the neurosurgeons at Niguarda Hospital, is passionate about disseminating his robotic stereotactic technique, based on the classical Talairach methodology. “Surgery has long been considered a treatment of last resort after patients have unsuccessfully tested combinations of antiepileptic medications for many years,” explained Cardinale. “However, after two drugs have been determined to be ineffective or intolerable, the chance of a third drug being effective is lower than 5%1. Surgery has long been shown in randomised controlled clinical trials to be superior over medical therapy in clinical and psychosocial outcomes2,3, not to mention the economic and social impact of a lifetime coping with severe impairment. Isn't it time that surgery became an early alternative, especially for young children who do not respond satisfactorily to one or two antiepileptic drugs?”
For many patients with epilepsy, intracerebral recordings are necessary for the definition of the epileptogenic zone (EZ). Stereoelectroencephalography (SEEG) is a procedure aimed at placing recording electrodes directly within brain structures, with a patient-tailored exploration strategy on the basis of non-invasive studies.
During SEEG, up to 20 electrodes are inserted deep within the brain, each with up to 18 electrical contacts along its length, to provide electrophysiological recordings of unmatched spatial density and accuracy. A retrospective evaluation of 81 electrode implantation procedures, carried out with the neuromate robot and frame-based patient registration, demonstrated a median application accuracy of 0.78 mm at the cortical entry point, the most risky zone of the trajectory4. These excellent accuracy figures have been further complemented with the introduction of the neurolocate registration system5.
Pre-operative planning
Dr. Cardinale co-registers a combination of multiple imaging datasets. 3D rotational angiography provides bone and vessel structures at a high resolution, while different magnetic resonance imaging (MRI) modalities allow the visualisation of parenchymal structures. The surgeon determines the surgical plan for inserting the electrodes, avoiding vessels. These imaging and planning steps are performed well in advance of the surgery.

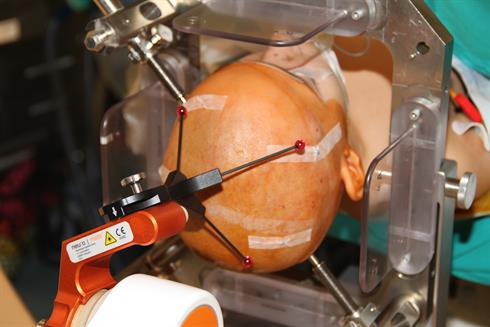
Dr Cardinale using the neuromate robot during an SEEG procedure
Surgery has long been considered a treatment of last resort after patients have unsuccessfully tested combinations of antiepileptic medications for many years. However, after two drugs have been determined to be ineffective or intolerable, the chance of a third drug being effective is lower than 5%1. Isn't it time that surgery became an early alternative, especially for young children who do not respond satisfactorily to one or two antiepileptic drugs?
Claudio Munari Epilepsy and Parkinson Surgery Centre (Italy)
Surgical procedure
On the day of the surgery, the patient, under general anaesthesia, has their head placed in the head holder mounted on the base of the neuromate robot and the O-arm® intraoperative imaging device is moved into position around the patient's head.
In image guided robotic surgery a key element of procedure accuracy is patient registration. Dr. Cardinale and his colleagues are using the neurolocate frameless registration system. The neurolocate module does not require any skin or bone anchored fiducials and enables intraoperative registration to be carried out using mobile X-Ray or computer tomography (CT), for example the Medtronic O-arm. The neurolocate technology is based on a fiducial marker that is mounted on the robot arm during intraoperative X-Ray or CT and Dr. Cardinale was instrumental in the development of the system. The team in Milan was able to demonstrate that neurolocate based registration can provide at least the same accuracy as the previously used framebased method, with the additional benefits of a comfortable, non invasive, easy to use workflow. With the neurolocate module the median application accuracy at the cortical entry point has been reported5 as 0.59 mm.
 Patient registration with the neurolocate module
Patient registration with the neurolocate module
The neuromate robot enables the precise and accurate positioning of the tool holder along a pre-planned trajectory, at a specified distance to the patient's skull and cerebral target. The surgeon percutaneously drills down to a depth corresponding to the inner surface of the skull. A monopolar coagulator is used to coagulate the dura mater. The surgeon mounts a hollow guiding screw into the drill hole through the robot guide, thus ensuring alignment with the planned trajectory. The robot arm is then moved into position for the next screw placement.
In the second phase of the surgery, the surgeon positions SEEG electrodes through the guiding screws. A rigid stylet is first inserted and retracted to create a tract. Then, the semi-rigid electrode is inserted. Various models of electrodes are available with a range of lengths and numbers of contacts. This entire process occurs under 2D X-ray control performed with the O-arm.

neuromate robot being used to position the drill guide
Post-operative care
Following the stereotactic electrode implantation, the surgical team immediately performs post-operative controls with an O-arm 3D scan, co-registered to the preoperative MRI, to provide precise localisation information on each contact of the SEEG electrodes. The electrodes are then tested for proper functioning, allowing their immediate replacement in case of failure.
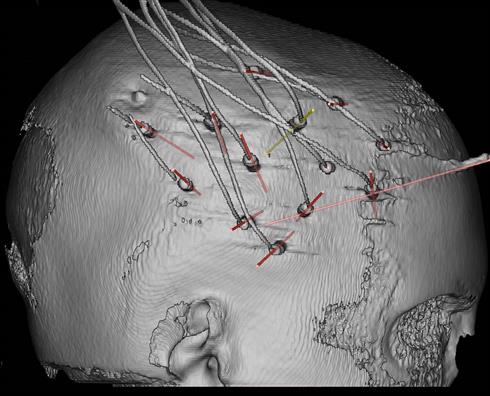
Electrodes in situ, as visualised by surgical planning software
The patient is later transferred into a video-EEG monitoring room and remains under constant observation for a period of five to fifteen days. Video and electrophysiological monitoring systems record several seizures, until a satisfactory assessment of the origin and spreading pattern of the seizures can be determined. The electrophysiologists also use electrical stimulations through the implanted electrodes to complete the definition of the EZ and to perform brain mapping. Most of the patients who undergo SEEG procedures are subsequently referred to surgical treatment, often tailored microsurgical resections aimed at removal of the epileptogenic zone, under MRI-based neuronavigation.
Discussion
Since the brain and especially the cortical surface are dense in blood vessels, image planning and precise implantation based on accurate visualisation of the vessels is essential. The stable neuromate robotic platform, driven by the surgeon through advanced surgical planning software, makes for a much more efficient technique for the delivery of multiple SEEG electrodes.
The total rate of SEEG related complications has been reported significantly lower compared to complication rates in other invasive monitoring techniques6. Dr. Cardinale ascribes this to the careful planning tailored to each patient, based on high resolution neuroimaging, and the great geometrical accuracy of the neuromate robot. He attributes the very low infection rate to the minimally invasive percutaneous approach.
In a recently published7 restrospective study of 742 SEEG procedures performed at Niguarda Hospital, the neurosurgical team observed that “since the introduction of the (neuromate) workflow, no major intracranial bleedings have occured, testifying that new technologies and a rigorous approach have made this invasive procedure even safer that in the past.”
References
(1) Kwan P, Brodie MJ. Early identification of refractory epilepsy. N. Engl. J. Med. 2000;342(5):314-9.
(2) Dwivedi R et al. Surgery for Drug-Resistant Epilepsy.Children. N. Engl. J. Med. 2017;377:1639–1647.
(3) Wiebe S et al. A randomized controlled trial of surgery for temporal-lobe epilepsy. The New England journal of medicine. 2001;345(5):311-318.
(4) Cardinale F et al. Stereoelectroencephalography: Surgical Methodology, Safety, and Stereotactic Application Accuracy in 500 Procedures. Neurosurgery 2013;72(3):353-366.
(5) Cardinale F et al. A new tool for touch-free patient registration for robot-assisted intracranial surgery: application accuracy from a phantom study and a retrospective surgical series. Neurosurg Focus 2017;42(5):E8
(6) Cossu M, Cardinale F. SEEG has the lowest rate of complications. Letter to the editor; J Neurosurg Volume 122, February 2015
(7) Cardinale F et al. Stereoelectroencephalography: retrospective analysis of 742 procedures in a single centre. Brain 2019;142:2688-2704
Please note that not all Renishaw products, their fields of application, relative accessories or combination thereof, are available in all countries.

